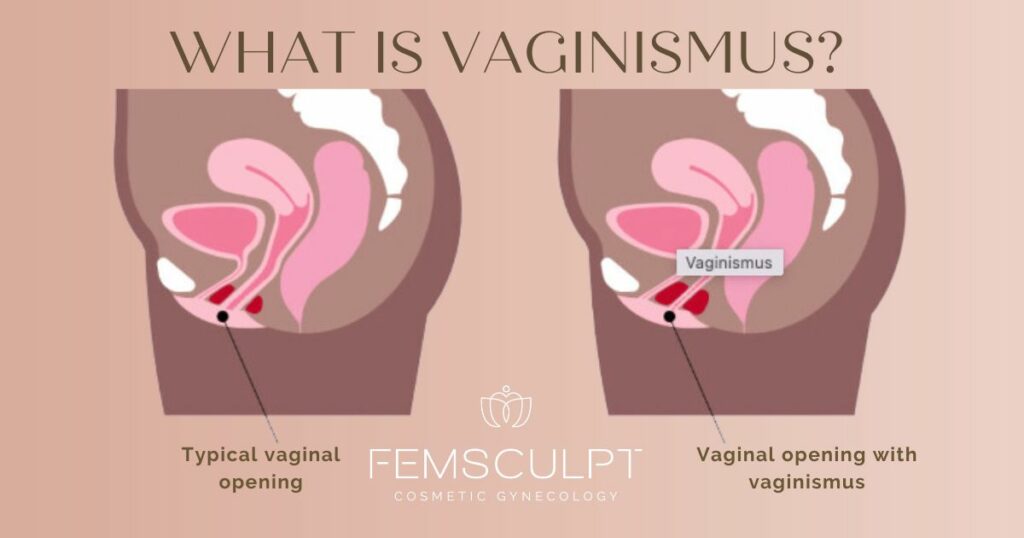
Vaginismus is a medical condition that causes the vaginal muscles tighten up involuntarily whenever you try anything like inserting any form of vaginal penetraion like a tampon, having sex, or even during a routine gyno exam. It can feel like a muscle reflex that just takes over and can be very uncomfortable.
This condition affects the perineal muscles, which are right beneath the skin, as well as the deeper muscles within the pelvic floor. If you’ve had pain during penetration before, it can make future attempts feel even more daunting. This is because the anticipation of pain can actually intensify your discomfort and lead to stronger muscle contractions, creating a cycle that further increases the pain or discomfort.
What Causes Vaginismus?
It’s not exactly clear what causes vaginismus. Estimates suggest that it affects between 1-7% of women. Unfortunately many women to struggle with using tampons, undergoing vaginal ultrasounds, gynecological exams, or even Pap smears without the aid of general anesthesia.
Personal experiences could play a role in the development of vaginismus. For instance, some women may have fears that sexual intercourse could be painful or harmful, or they might worry about their anatomy being abnormal. Additionally, some cultural or religious beliefes may also have an impact such as specific views about intimacy. Life’s stresses, along with mental health challenges like anxiety, depression, and a history of trauma, including childhood abuse or sexual violence, can also be contributing factors.
Physical Factors Behind Vaginismus

When it comes to vaginismus, it’s important that your gynecologist consider any physical factors or underlying causes that might be contributing to your vaginismus. Identifying these can ensure that you receive the most appropriate care and avoid spending time on treatments that might not address the underlying issue. Some physical conditions include:
- Endometriosis: This condition could be a key factor in vaginismus. It’s often linked to menstrual pain, discomfort during bowel movements, pelvic pain outside of your period, and pain during sexual intercourse.
- Recurrent Infections: Frequent antibiotic use for other infections can sometimes lead to recurring vulvo-vaginal thrush. This can cause soreness in the skin, making penetration painful.
- Sexually Transmitted Infections (STIs): Certain STIs, like vulval warts or herpes, might lead to what’s known as secondary vaginismus. This can happen if there’s ongoing pain even after the STI has been treated.
- Pudendal Nerve Sensitivity: Increased sensitivity or pain in the pudendal nerve, which affects the pelvic and perineal areas, can also be a contributing factor.
- Skin Conditions of the Vulva: Conditions like Lichen sclerosus, eczema, dermatitis, or psoriasis can impact the skin in the vulval area, leading to discomfort.
- Changes Post-Menopause: Skin changes due to menopause, early menopause, or menopause following breast cancer treatment can also play a role. Other factors like irregular or absent periods and long-term use of birth control pills can affect skin integrity due to changes in estrogen levels. This can lead to thinning of the skin, dryness, redness, splitting, and irritation, all of which might make penetration painful and trigger vaginismus.
How is Vaginismus Treated?
Treating vaginismus is often multifaceted, tailored to each individual’s unique experiences and needs. Some women may require one or multiple interventions.
Pelvic Floor Physical Therapy
A specialized physical therapist can help you learn how to control and relax your pelvic floor muscles. Techniques often include exercises to stretch and strengthen these muscles, sometimes using vaginal dilators to gradually accustom the area to penetration.
Psychological Support
Since vaginismus can have psychological components, therapy can be immensely helpful. Cognitive-behavioral therapy (CBT) is commonly used to address any underlying fears or anxieties related to penetration. This therapy helps in breaking the cycle of pain and fear by changing thought patterns and behaviors.
Sex Therapy or Counseling
exploring and discussing sexual health and intimacy with a counselor or sex therapist can be beneficial. This can also be an opportunity for couples to address any issues affecting their sexual relationship.
Medications
In certain cases, medications may be prescribed. These can include muscle relaxants, pain relievers, suppositories or even topical anesthetics to reduce discomfort during physical therapy exercises or intercourse.
Neuromodulator Injections
For more severe cases, neuromodulator injections into the pelvic floor muscles might be considered. This can temporarily relieve muscle tension, making it easier to proceed with physical therapy.
PRP Injections
PRP injections, or platelet rich plasma therapy, can also help provide relief from vaginismus.
Navigating the complexities of women’s gynecological health and intimate wellness can be a deeply personal and sometimes challenging journey. If you’re seeking guidance, support, and expert care, Dr. Sue Kafali at Femsculpt Cosmetic Gynecology is here to help. Renowned for her expertise in cosmetic gynecology and a deep commitment to women’s health, Dr. Kafali offers a compassionate approach tailored to your unique needs and goals.
Contact our office to schedule a consultation with Dr. Sue Kafali at Femsculpt Cosmetic Gynecology today. Together, we can help you navigate your journey toward a healthy life, and renewed confidence.
About Dr. Sue Kafali

Board-Certified Cosmetic Gynecologist and top labiaplasty surgeon Dr. Sue Kafali of FemSculpt Cosmetic Gynecology specializes in vaginal rejuvenation surgery & intimate wellness in Chicago, Illinois. For a complimentary consultation with Dr. Sue Kafali, contact our office today.
